By Jan Bowers, contributing writer
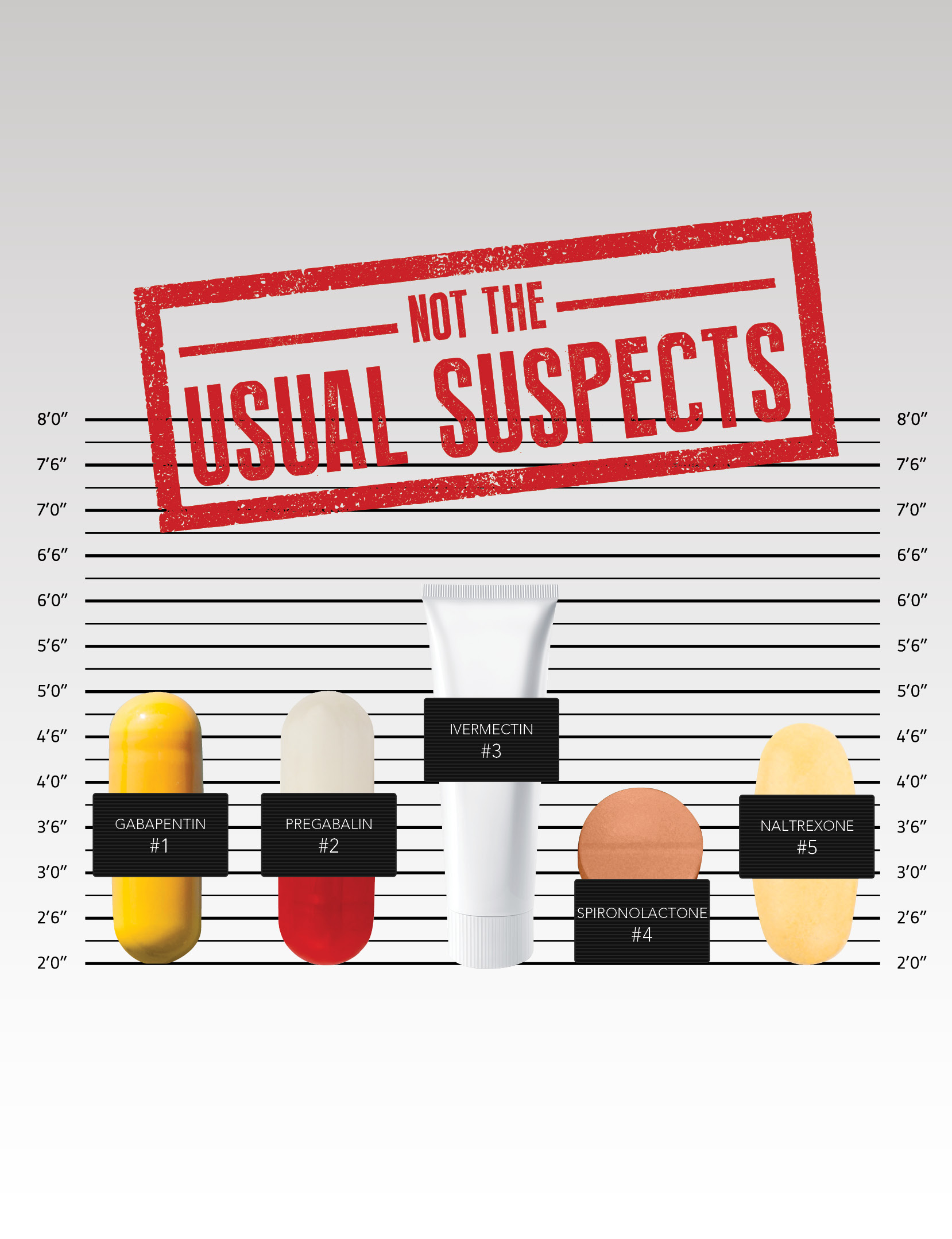
Young dermatologists quickly become familiar with mainstays of treatment such as antibiotics, corticosteroids, and antihistamines. However, when those therapies fail, or when conditions dictate a novel approach, less common agents can play a key role in the treatment of acne, rosacea, pruritus, and other skin disorders. Dermatology World spoke with four dermatologists about their experiences and research in treating selected patients with:
- Gabapentin and pregabalin
- Ivermectin
- Spironolactone
- Naltrexone
Attacking chronic itch
Two anticonvulsant medications that have been used to manage chronic pain are also proving effective in the treatment of selected types of chronic itch: gabapentin and pregabalin.
“Chronic pain and chronic itch have a lot of similarities,” said Gil Yosipovitch, MD, professor of dermatology at the University of Miami Miller School of Medicine and director of the Miami Itch Center. “This is one of the mainstay treatments that I use for patients who have chronic itch of different types.”
Dr. Yosipovitch cited neuropathic itch, a result of nerve damage, and itch caused by neural sensitization as two types that respond well to gabapentin and pregabalin. “People with atopic dermatitis, for example, have a neural sensitization phenomenon, meaning the nerves are hyperactive — they’re very sensitive, and they fire more than a normal nerve,” he explained. “What the gabaergic drugs do is reduce that hyperactivity. They were designed initially for epilepsy, where there’s a lot of electric activity of the nerves. They’re now prescribed for many different kinds of pain, so it makes sense to use them in chronic itch associated with neural sensitization, as well as for neuropathic itch.”
Efficacy
In a clinical review of the mechanism of and therapeutic approaches to itch (J Allergy Clin Immunol. 2018;142(5):1375-139), Dr. Yosipovitch listed prurigo nodularis, postburn pruritus, uremic pruritus, and paraneoplastic pruritus, in addition to neuropathic itch, as indications for the use of anticonvulsant systemic therapies. Other conditions shown to respond to these drugs, according to a review of published studies (J Am Acad Dermatol. 2016;75:619-25), include brachioradial pruritus, notalgia paresthetica, and scalp dysesthesia, among others. The JAAD authors noted that among the conditions studied, uremic pruritus appeared to be the most responsive to these agents.
The gabaergic drugs work on interneurons, an inhibitory system in the spinal cord that may also be in the brain, Dr. Yosipovitch explained. “They most probably inhibit the overactivity of the nerve. They don’t inhibit the nerves from acting; they don’t block all transmission. However, the intensity of the transmission goes down significantly. They don’t inhibit itch specifically; rather, they work on spinal nerve fibers, which can transmit both itch and pain.”
Dosing
Dosing depends on the age of the patient and the underlying conditions — and pregabalin is given less frequently and at lower doses than gabapentin, Dr. Yosipovitch said. For gabapentin, “I start with a low dose of 300 milligrams and increase it gradually every two days by another [300 mg] tablet. I usually start it at nighttime, because this drug initially causes significant sleepiness.” In patients with kidney failure who are on dialysis, “you give low doses, like three times a week, after dialysis. In younger folks that I see sometimes who have significant neuropathic damage, I start with 600 milligrams.”
Gabapentin is usually given three or four times a day, but “with pregabalin it’s only twice a day, and the doses are much lower. The maximum dose I usually give is 300 milligrams a day — it could be 400 — and the minimum could be 25 to 50 milligrams.” Pregabalin is easier to use because it requires fewer doses, Dr. Yosipovitch pointed out, but “it’s more expensive, so insurance companies would prefer that we don’t allow a lot of patients to be on pregabalin without first using gabapentin.” Another factor in choosing between the two agents is that some patients who fail gabapentin will respond to pregabalin, and vice versa. “I don’t have any explanation in terms of pharmacology. The drugs work on the same receptors,” Dr. Yosipovitch said. “There are no studies that compare the two head to head. It just shows that our human bodies are unique.”
Side effects
In addition to drowsiness, adverse events include dizziness and swelling of the legs, Dr. Yosipovitch noted. “The swelling is not putting patients at risk in any way, but it’s important to understand. In some patients, there is constipation and GI complaints, but overall, these two drugs are now used by millions of patients.” As one of the first dermatologists to use gabaergic drugs to manage itch, Dr. Yosipovitch said that unlike the situation 10 years ago when, “I could count the number of dermatologists using them on two hands, now, I would say that most dermatologists are at least aware of them.” Some are hesitant to give patients doses above 300 milligrams, “but experts usually give higher doses that go up to 3 grams and more. Patients come to me and say, ‘they gave me gabapentin, one pill,’ so 100 or 300 milligrams. That’s not a dose that would usually work for these types of itch, so that’s one of the challenges.”