By Allison Evans, assistant managing editor
A physician’s job, pared down to its most simplistic form, is to take care of patients. Some would argue that to take the best care of patients, physicians must also take care of themselves. While the idea of 30 minutes of activity most days a week seems achievable — even practical — why is it so hard for many Americans to meet the recommended activity guidelines? One of the biggest obstacles cited is finding the time and energy for exercise. For physicians, this struggle continues to escalate as administrative and regulatory hurdles have increased the load of a workday to capacity.
Physicians — like many Americans — struggle to balance the increasingly numerous demands of modern life with the growing body of evidence indicating the significance that movement plays in long-term health. This month, Dermatology World explores the relationship between fitness and physician and talks to dermatologists who love exercise, those who don’t, and those who fall somewhere in between. They share experiences getting and staying in shape, as well as how staying fit may make them better physicians.
Active physician, active patient?
Research suggests that active physicians are more likely to provide more credible and motivating counsel to their patients. Additionally, research shows that physicians who engage in physical activity are more likely to counsel patients about its significance. While much of this research focuses on counseling from primary care physicians, it is clear that lifestyle risks play an increasingly important role in managing dermatologic conditions as well.
In a recent JAAD article, ‘Skin changes in the obese patient,’ the authors note that the consequences of obesity in the skin are underestimated. Obesity is associated with a variety of skin manifestations, including acanthosis nigricans, acrochordons, keratosis pilaris, striae distensae, cellulite, and palmoplantar keratoderma-plantar hyperkeratosis. It also impacts collagen structure, wound healing, sweat glands, and more, and is associated with increased incidence of chronic dermatoses like hidradenitis suppurativa, psoriasis, and rosacea (https://doi.org/10.1016/j.jaad.2018.12.070).
All physicians may soon play a more significant role in weight and lifestyle preventive care as the global economic and social impact of inactivity is better understood. The Heavy Burden of Obesity released by the Organisation for Economic Co-operation and Development (OECD) found that more than half of the population is now overweight in 34 out of 36 OECD countries, including the U.S., countries in the European Union, and other high-income countries. Additionally, the report found that one-third of people do not get enough physical activity. (View the report at www.oecd.org/health/the-heavy-burden-of-obesity-67450d67-en.htm.) The data add up to a future in which physician counsel on the importance of fitness — both from primary care and specialists — will become paramount.
Rx for exercise
According to patients surveyed from a university family practice, 70% said they would be more willing to exercise if their physicians also exercised regularly. Nearly 85% of the patients were more willing to comply if their physicians gave them a written exercise prescription (Clin J Sport Med. 1996 Apr;6(2):112-8).
Oregon dermatologist Douglas Naversen, MD, does just that. He attempts to motivate patients with a script that reads, “I am going to write you a special prescription for a medicine that will do all of the following: Lower blood pressure, blood sugar and weight; improve cholesterol, sleep, bone and heart health, and decrease the risk of cancer. Does this prescription really exist? Yes — but there is just one catch: You’ll need ___ minutes each day to take it. Yes, the ‘medicine’ I am talking about is exercise.”
Dr. Naversen writes the prescription for his patients struggling to lose weight, including those with dermatologic conditions such as psoriasis, hidradenitis suppurativa, and intertrigo. “We know that people with severe psoriasis have double the risk of heart attack and stroke. I will get them started on a walking and exercise program and refer them to their family doctor or internist to be screened for risk factors for cardiovascular disease,” he explained. “If we put the patient on a biologic and get their severe psoriasis under remission, their risk goes back to normal.”
Although Dr. Naversen admits the yield is low, some patients surprise him and lose 15 to 20 pounds over the next year. “The record: One husband and wife team lost a combined 110 pounds in one year after my cajoling and prescription for exercise.”
As a physician, physical fitness has added significance for Dr. Naversen. “It gives me clout with my patients. Since everyone knows I am a runner, it helps attract the patients I like to treat best — aerobic people with an active lifestyle who like to take care of their bodies and their skin.”
Working out to work better
Warren R. Heymann, MD, head of the division of dermatology at Cooper Medical School of Rowan University, believes that his fitness regimen helps him be a better physician. As someone who has struggled to ditch a few pounds and get healthier, he is better able to empathize with patients who struggle with weight loss.
“It’s easier to encourage people, let’s say, who have HS or psoriasis, to get to their optimal weight. I’m not being hypocritical asking people to do something that I haven’t had to do myself; I know that it’s doable and takes a lot of determination. It would be like a smoker telling someone not to smoke.”
According to a 2016 survey by the Cardiovascular Research Foundation, of primarily cardiologists, only 22% of respondents said they had received any formal education or training about prescribing exercise.
Despite the body of evidence highlighting the potential impact of physicians as role models when it comes to fitness, and data that show most physicians support promoting exercise, there is still little emphasis and direction on how physicians should promote and prescribe exercise in practice (doi:10.1016/0091-7435(92)90070-x).
A big, fat lie
Read about how Dr. Heymann changed his lifestyle and his commentary on presidential weight gain at staging.aad.org/dw/dw-insights-and-inquiries/medical-dermatology/a-big-fat-lie.
A patient counsels a physician
“When I was in my early 40s, I walked into a patient’s room and he said, ‘Hey, doc, packing on the pounds, aren’t you?’ And I replied, ‘Good morning to you,’” said Dr. Heymann. Sheepishly, he admitted that he had in fact gained some weight.
“You better take the weight off now. Once you’re over 50, your knees will be shot, and there’s no way you’ll get it off,” the patient continued. After this unusual encounter, Dr. Heymann — like many others — wondered when he was supposed to find the time to exercise when he “worked like a fiend,” and had young kids at home.
After thinking about it more, Dr. Heymann knew his patient had been right. He decided to take the weight off and start exercising each morning. “I set my clock for 5:10 a.m. and got a half-hour of exercise in nearly every day — using the elliptical machine or taking a brisk two-mile walk. If I don’t do it first thing in the morning, there’s a good chance I’m not going to get to it.”
No love loss
Fast forward more than 20 years later and Dr. Heymann still maintains his workout regimen most days of the week. Although he is nothing if not candid about his lack of passion for exercise.
“As I got older, I added a weekly weight training session with a personal trainer. We meet at 6 a.m. for 30 minutes. The happiest minute of my week is 6:31 a.m. when the torture ends,” he said.
“I can’t say I’m passionate about exercise. It’s become part of my routine, and it’s become part of my life, but I’d be lying if I said I love it. This was something I needed to do,” he explained.
“You always hear about a ‘runner’s high,’ or sense of euphoria. I don’t get this feeling. When my exercise is over, I’m happy — euphoric, even — because it’s over.”
A passion for the burn
Some dermatologists have a true love for fitness. Dr. Naversen hasn’t missed a day of running in over two years and two months. Since he turned 70 in October 2018, he has remained undefeated in his age group for the year in all of his Oregon, California, and Hawaii running races. After running nearly 30 marathons, he took a year and half off to recover from knee injuries. “I became a couch potato and enjoyed it,” he said. But he returned to marathon running in April 2019 at the Eugene, Oregon Marathon. Having done only one long training run beforehand, he won his age group and qualified for the Boston Marathon with 27 minutes to spare.
Dermatologist on the run
Read more about Dr. Naversen’s passion for running and how it has played a role in his professional life at staging.aad.org/dw/monthly/2018/august/dermatologist-on-the-run.
Jeremy Bordeaux, MD, MPH, has found a home in the CrossFit community, where he enjoys making connections with fellow dermatologists and staying in shape. Like Dr. Heymann, Dr. Bordeaux is up at 5 a.m. every morning to ensure he prioritizes the workout. Even at that early hour, the social aspect of CrossFit is part of what he loves most. “I have a close social community of friends that I work out with — we challenge each other.” He and a few dedicated colleagues have even organized CrossFit workouts for die-hards and newbies alike at dermatology meetings around the country.
Aside from the sense of community and unique physical challenges offered by CrossFit culture, Dr. Bordeaux says that the program also fulfills an underlying instinct common to most physicians — the impulse to continue learning. “Within the CrossFit world, you’re always learning different things, like how to climb a rope without your legs, do handstand push-ups, or how to jump a rope twice. There are all these different things that you’re constantly learning, which I think is analogous to our specialty. As a dermatologist, I feel like I’m continually learning new things and pushing myself.”
Exercise as stress-buster
While some dermatologists demonstrate an awe-inspiring commitment to fitness, this certainly isn’t the norm. For Ohio dermatologist Jennifer Lucas, MD, fitness has always been a part of her life, but her relationship to the intensity of her workouts has waxed and waned over the years. She used exercise as a way out of a particularly difficult period in life that otherwise would have been overwhelming.
“I exercise because it clears my head and gives me peace and calm amidst all the chaos and stress of life. In the morning, I exercise to wake myself up and start the workday with focus and energy. In the afternoon, I exercise to clear my head and wash out all the stress and pressures of the day. When I exercise, I can deal with life and all that comes at me with much more poise and grace.”
According to Medscape’s Dermatologist Lifestyle, Happiness & Burnout Report 2019, dermatologists cope with burnout with a mix of positive and destructive behaviors. More than half (53%) of dermatologists cope with burnout through exercise. Interestingly, however, the scale is balanced when looking at the rest of the numbers: 26% drink alcohol, 24% eat junk food, and 23% binge eat.
New York dermatologist Elyse Love, MD, also believes fitness makes her a better physician. “I find that I am more anxious, more easily bothered, and more easily frazzled when I do not work out. My daily workout routine allows me to have a more patient and friendly bedside manner.”
Exercise for the adventurer
For New York dermatologist and dermatologic surgeon Ellen Marmur, MD, physical fitness is part of her daily routine. “Exercise is a form of meditation and focus; it cleanses the mind and skin. Exercise boosts my clarity and energy and makes me a better leader,” she said.
Additionally, Dr. Marmur finds fitness allows her to better connect with her patients. “My patients comment on my fitness and love to share their adventures with me. We inspire each other to stay active!”
Dr. Marmur also combined her love of adventure with her passion for educating others about skin cancer. The result: The inaugural Skin Cancer, Take a Hike!™ climb up Mt. Kilimanjaro in 2014. “I created Skin Cancer, Take a Hike! to raise awareness about sun protection and skin cancer prevention while living your life to the maximum and enjoying the outdoors.”
With the program in its fifth year, dermatologists and patients have taken this hike viral from the summit of Mt. Kilimanjaro to local peaks all over the country and the world, Dr. Marmur said. The latest hike, which took place in July, was in the volcanic lava fields of Iceland (Laugavegur trail). “Our bodies were made to move, and exercise and skin care are essential for our best health.”
Skin Cancer, Take a Hike!™
Join a hike in your area (or around the world) or donate to an upcoming hike at staging.aad.org/skin-cancer-take-a-hike.
Keeping it fresh
There’s something about the beginning of a new year that makes starting a sparkling new workout routine doable. But why is it that so few of those who embark on the notoriously flimsy fitness resolution can maintain it? One strategy may be to diversify your exercise portfolio to elude boredom.
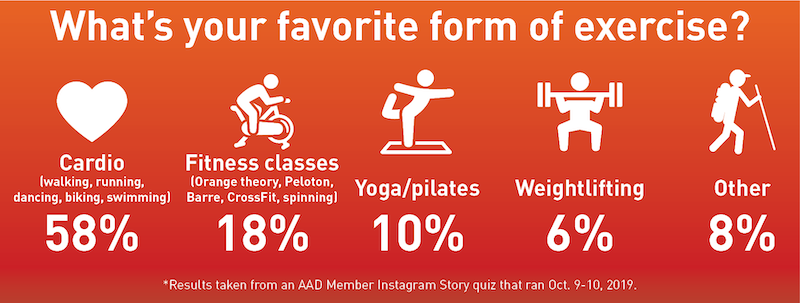
According to the American College of Sport Medicine’s Top 20 Worldwide Fitness Trends for 2019 report, group training was ranked as the No. 2 fitness trend. (See the sidebar for the top 10 fitness trends.) Notably, the report differentiates between a “trend” and a “fad.” A trend is defined as a “general development or change in situation or in the way people are behaving,” while a fad is defined as “a fashion that is taken up with great enthusiasm for a brief period.”
Dr. Lucas takes part in a variety of fitness programs such as Rise Nation, Peloton, boxing, personal training, and yoga. Many fitness trends and/or fads have popped up around the country over the years, including hot yoga (or goat yoga), CrossFit, Orangetheory, Peloton, and Rise Nation. However, it’s likely that more people will be using a combination of group workouts to eschew boredom and meet their fitness goals making these oft-described fads part of a growing trend.
Dr. Love changes her workout routine with the seasons. “I think mixing things up is how I’m able to sustain my long-term commitment to fitness. There’s no reason that fitness should be boring, and it’s also good for the body to move in different forms and rhythms.”
The pay off
“I’m exercising because I want to be around a long time, and I want to be in reasonably good health. I’m not trying to set any records. I’m trying to take care of myself, and the benefits of doing that are of manifold,” Dr. Heymann said.
“I want to stay healthy. I had my last child at 40, which means I’ll be old by the time she has kids, and I want to be able to keep up with them,” Dr. Bordeaux said. If you don’t take care of yourself, you can’t take care of your family and your patients.”
Exercise is work — especially when EHRs, prior authorizations, mountains of journal reading, not to mention family commitments eat up the bulk of a day or week. Unlike some of a physician’s daily tasks, exercise is an investment that pays dividends not only to oneself, but potentially to a community of patients as well. “Exercise is symbolic of my potential within my career. It reminds me of the rewards of consistency and sustainable hard work,” Dr. Love said.
