By Emily Margosian, assistant editor
A patient sitting in a dental chair might expect a number of things. An uneventful tooth cleaning, or an unenviable root canal. However, they may also anticipate something new: Botox.
Scope of practice remains an ongoing area of focus for many dermatologists concerned about the quality and safety of dermatologic care offered by other health care professionals. In 2019 alone, the American Academy of Dermatology Association (AADA) tracked over 70 different bills across the country relating to non-physician scope of practice affecting the practice of dermatology, according to Lisa Albany, JD, AADA director of state policy. “The AADA worked in coordination with state medical societies and state dermatology societies to oppose many of these dangerous bills.”
The year 2020, however, has thus far proved to be an extraordinary year with its own unforeseen set of challenges. As the COVID-19 pandemic continues, many states have relaxed scope of practice restrictions for non-physicians to help address workforce shortages during the crisis. While potentially beneficial in the short-term, “Even if these relaxations really are temporary, and states go back to the status quo, we will still face challenges,” explained Victoria Pasko, AADA assistant director of state policy. “We anticipate expanded scope of practice laws that have been temporarily authorized to address the COVID-19 pandemic will be used as an argument to permanently expand state scope of practice laws in the future.”
While what lies ahead remains uncertain, this month Dermatology World presents a snapshot of the current state of scope of practice with the following providers:
• Nurse practitioners
• Physician assistants
• Optometrists
• Naturopaths
• Dentists
Nurse practitioners
In the United States, approximately 25 states authorize advanced practice registered nurses (APRNs), including nurse practitioners, to practice independently. Of these, 10 states allow “transition to practice” whereby APRNs must complete a certain number of hours or years of collaborative or supervised practice with a physician or non-physician before practicing independently. The period ranges from less than a year (1,040 hours in South Dakota) to five years (Virginia).
Full practice: Alaska, Arizona, Colorado, Connecticut, Hawaii, Idaho, Iowa, Maine, Maryland, Minnesota, Montana, Nebraska, Nevada, New Hampshire, New Mexico, North Dakota, Oregon, Rhode Island, South Dakota, Vermont, Washington, Washington D.C., Wyoming.
Transition to practice: Delaware, Virginia, West Virginia.
Source: American Association of Nurse Practitioners
Legislation
Most legislation regarding nurse practitioners in 2019 fell into three categories:
● Authorizing NPs to practice independently
● Transition to practice
● Substituting supervision for collaboration
However, in a key victory for dermatologists, nurse practitioners did not gain independent practice in any state in 2019. The AADA and state dermatology societies successfully opposed NP independent practice legislation in California, Florida, Mississippi, Missouri, Pennsylvania, and Texas.
Mississippi offered dermatologists a unique scope of practice success story. In response to increased efforts from state NPs to seek independent practice, in 2019 the Mississippi State Medical Association (MSMA) launched a State Scope of Practice Partnership (SSOPP) campaign through the use of a grant from the AMA Scope of Practice Partnership (SOPP), of which the AADA is a steering committee member. Chaired by Mississippi dermatologist Sabra Sullivan, MD, PhD, the campaign was intended “to further strengthen the voice of physicians and underscore the critical role physicians play in leading the medical care team.”
Making use of billboards, social media hashtags, commercials, and significant grassroots efforts, the campaign’s multi-pronged push successfully resulted in Mississippi Gov. Phil Bryant’s decision to retain Medicare’s physician supervision requirements for certified registered nurse anesthetists, citing that “prudence dictates I defer to the judgement and experience of expert physician boards and associations on matters of public health and safety.”
Additionally, proposed transition to practice legislation in Indiana that would have allowed APRNs to practice independently after collaborating with another health care practitioner (not necessarily a physician), failed. The AADA and Indiana Academy of Dermatology (IAD) worked together to draft dermatologist testimony for legislators that contributed to the bill’s defeat. The AADA also successfully opposed legislation in Kansas that would have removed the collaborative practice agreement between an APRN and a physician, as well as the legal distinction between a medical diagnosis and nursing diagnosis.
What’s coming up in 2020?
As of July 1, Florida will be the latest state to allow NPs to practice independently. While California, Louisiana, Massachusetts, Missouri, Nebraska, New Jersey, Oklahoma, and Tennessee are considering similar legislation, it is unlikely the bills will be taken up during the current legislative session due to the ongoing COVID-19 pandemic.
How has the law changed with COVID-19?
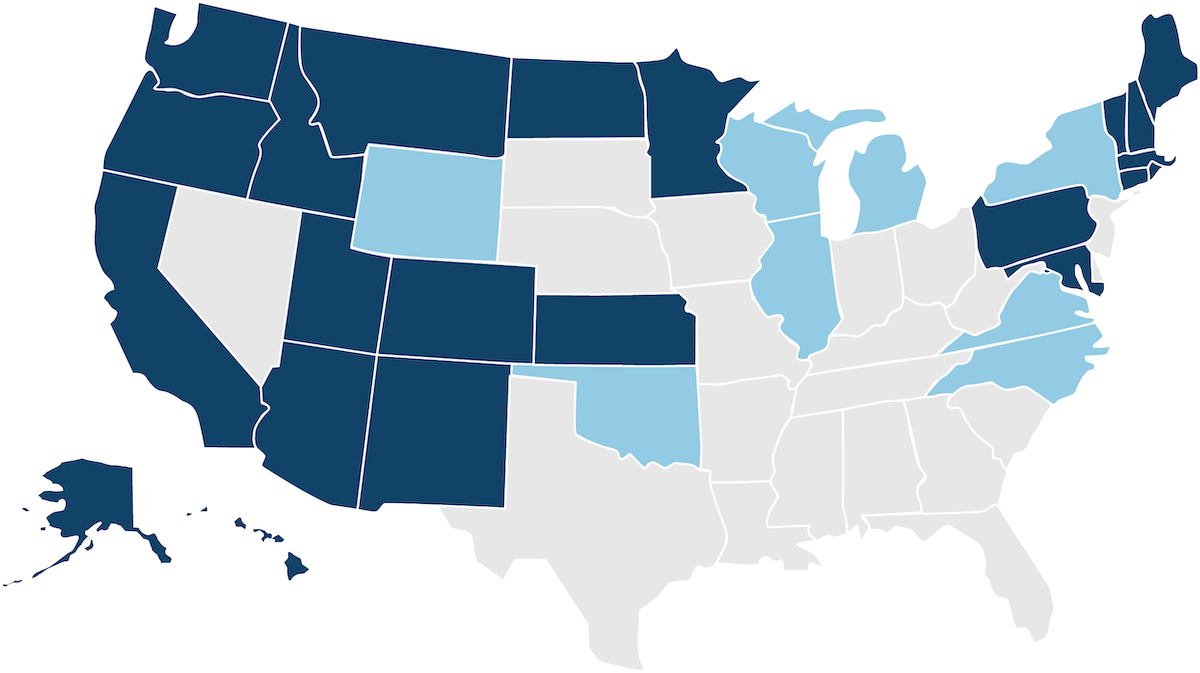
Due to the COVID-19 crisis, several states have relaxed scope of practice requirements for nurse practitioners to either partially or fully suspend supervision requirements — a decision that has received public praise from nursing boards nationwide. See the map below for a breakdown of which states have experienced changes to NP scope of practice due to the pandemic.
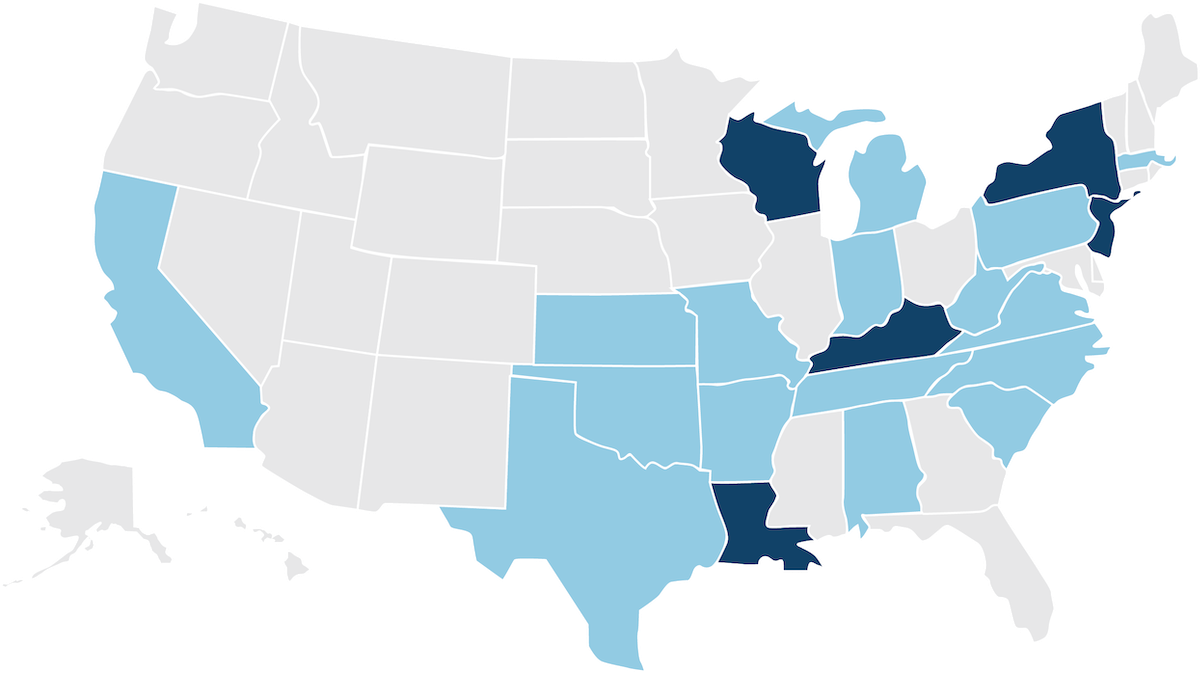
Temporary suspension of all practice agreements: Kentucky, Louisiana, New Jersey, New York, Wisconsin.
Temporary suspension of select practice agreements: Alabama, Arkansas, California, Indiana, Kansas, Massachusetts, Michigan, Missouri, North Carolina, Oklahoma, Pennsylvania, South Carolina, Tennessee, Texas, Virginia, West Virginia.
*As of Apr. 28.
Physician assistants
Currently, a majority of states (40) require physician supervision of physician assistants (PAs), in addition to limiting the number of PAs a physician can supervise or collaborate with. In eight states, PAs are subject to collaborative agreements with physicians, while two states — New Mexico and Michigan — allow for alternative arrangements. New Mexico calls for supervision of PAs with less than three years of clinical experience and for specialty care PAs, while Michigan authorizes PAs to work under a participating physician. In nearly all states (48), PA scope of practice is determined with the supervising or collaborating physician at the practice site.
Legislation
Numerous states introduced legislation in 2019 that would amend PA scope of practice. Most of this legislation included language on:
● Eliminating supervision requirements and replacing supervision with collaboration
● Authorizing independent practice
● Increasing supervision ratios
What were the results? In coordination with the American Medical Association (AMA), as well as state medical and dermatology societies, the AADA successfully defeated efforts to expand PA scope of practice in six states: Illinois, Louisiana, Maine, Montana, Nevada, and Oregon. “The AADA stays in constant communication with state medical societies as they conduct discussions and negotiations with the physician assistants and legislatures,” explained Pasko.
In Louisiana, the AADA worked in coordination with the Louisiana Dermatology Society and Louisiana State Medical Society to successfully oppose legislation that would have removed supervision of PAs. The bill was ultimately stripped of all provisions to change the supervisory relationship and retained existing law.
In Connecticut, the AADA assisted state dermatologic societies to oppose efforts of PAs to expand scope of practice. Although the law was ultimately amended to allow PAs to work in a collaborative relationship with a physician, it retains the requirement that PAs provide patient services under the supervision and direction of a licensed physician.
What’s coming up in 2020?
The AADA is currently tracking 2020 legislation that would expand PA scope of practice in nearly 40 states.
In the Midwest, Wisconsin is considering legislation that would eliminate the formal supervisory relationship between physicians and PAs, while Iowa recently enacted new legislation in March that allows PAs to prescribe medication.
In the northeast, Maine also enacted legislation in March that removed supervision requirements for PAs. While the bill requires PAs with less than 4,000 clinical hours to practice in a collaborative agreement with a physician, those with more than 4,000 hours are now authorized to be the primary clinical provider in practices that do not include a physician partner.
As a result of opposition from the Oklahoma State Medical Association (OSMA), the AADA, and medical specialty organizations, legislators in Oklahoma removed language from legislation that would have eliminated the formal supervisory relationship between physicians and PAs. The language that passed both the House and Senate would prohibit PAs from providing “health care services independent of physician supervision.” Supervision would include overseeing or delegating the medical services rendered by a PA through a practice agreement between a physician (MD/DO) performing procedures or directly or indirectly involved with the treatment of a patient.
How has the law changed with COVID-19?
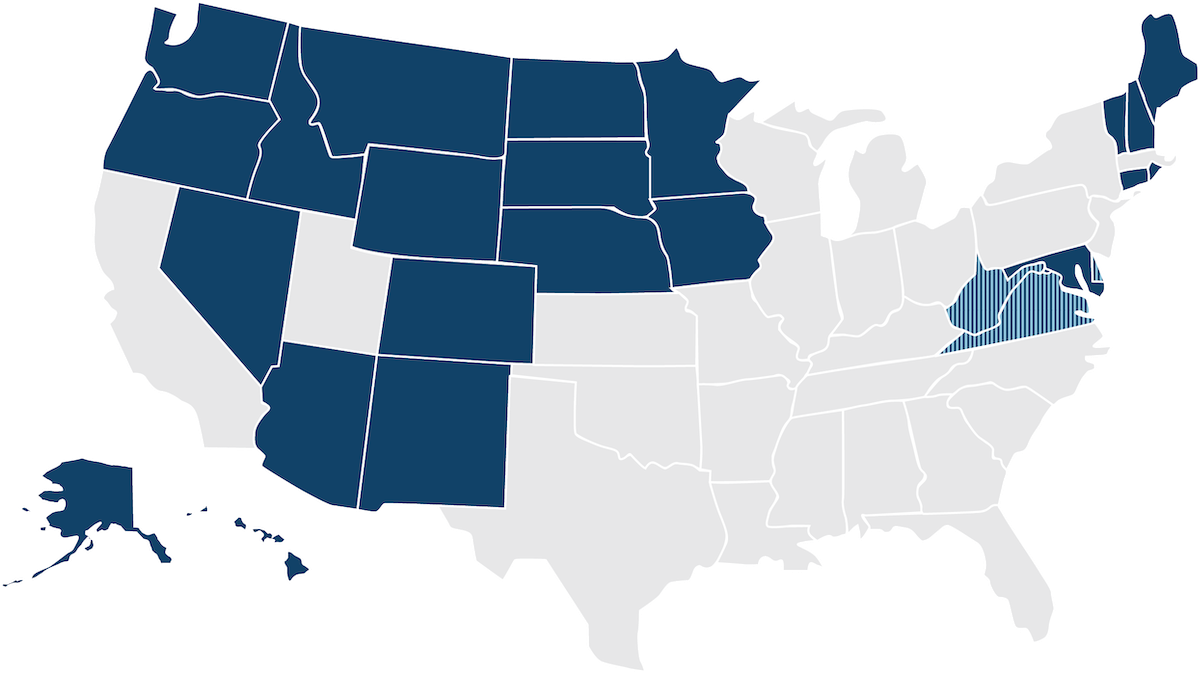
Due to the COVID-19 crisis, several states have relaxed scope of practice requirements for physician assistants to either partially or fully suspend supervision requirements. In response, the American Academy of Physician Assistants (AAPA) has since called for further easing of scope of practice restrictions, requesting that governors in all states waive physician supervision or collaboration requirements for PAs during a declared public health emergency or disaster. See the map below for a breakdown of which states have experienced changes to PA scope of practice due to the pandemic.
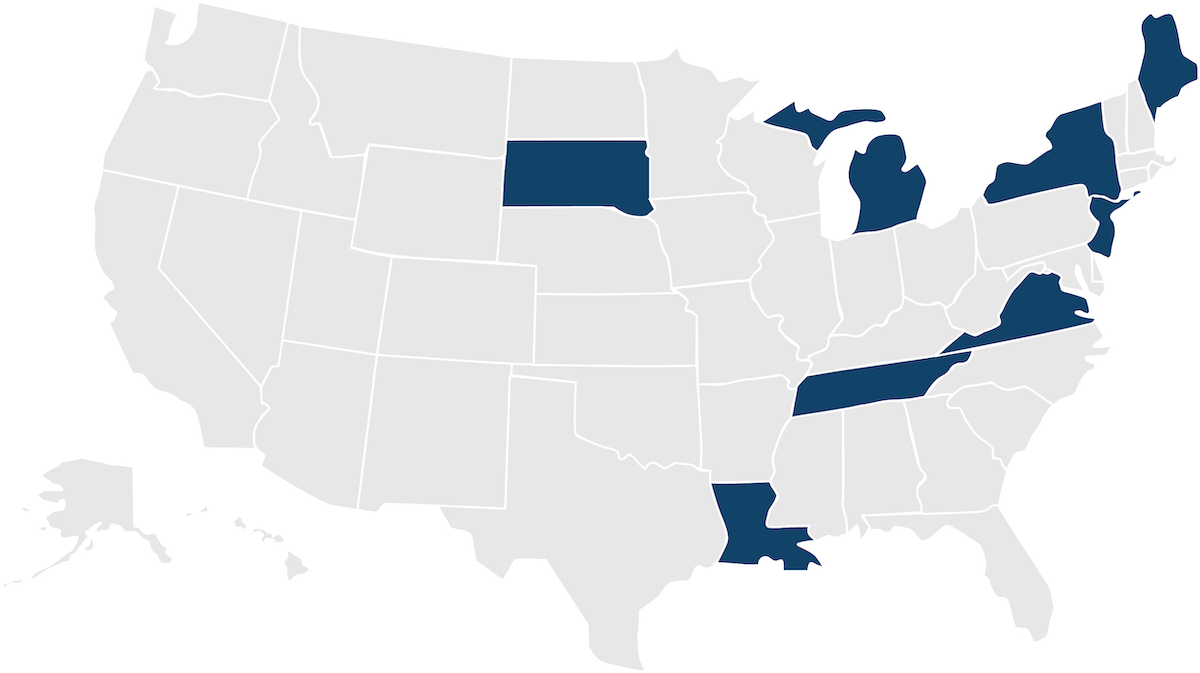
Suspended or waived supervision requirements by executive order: Maine, Michigan, New Jersey, New York, Louisiana, South Dakota, Tennessee, Virginia.
*As of April 28.